MD Curriculum
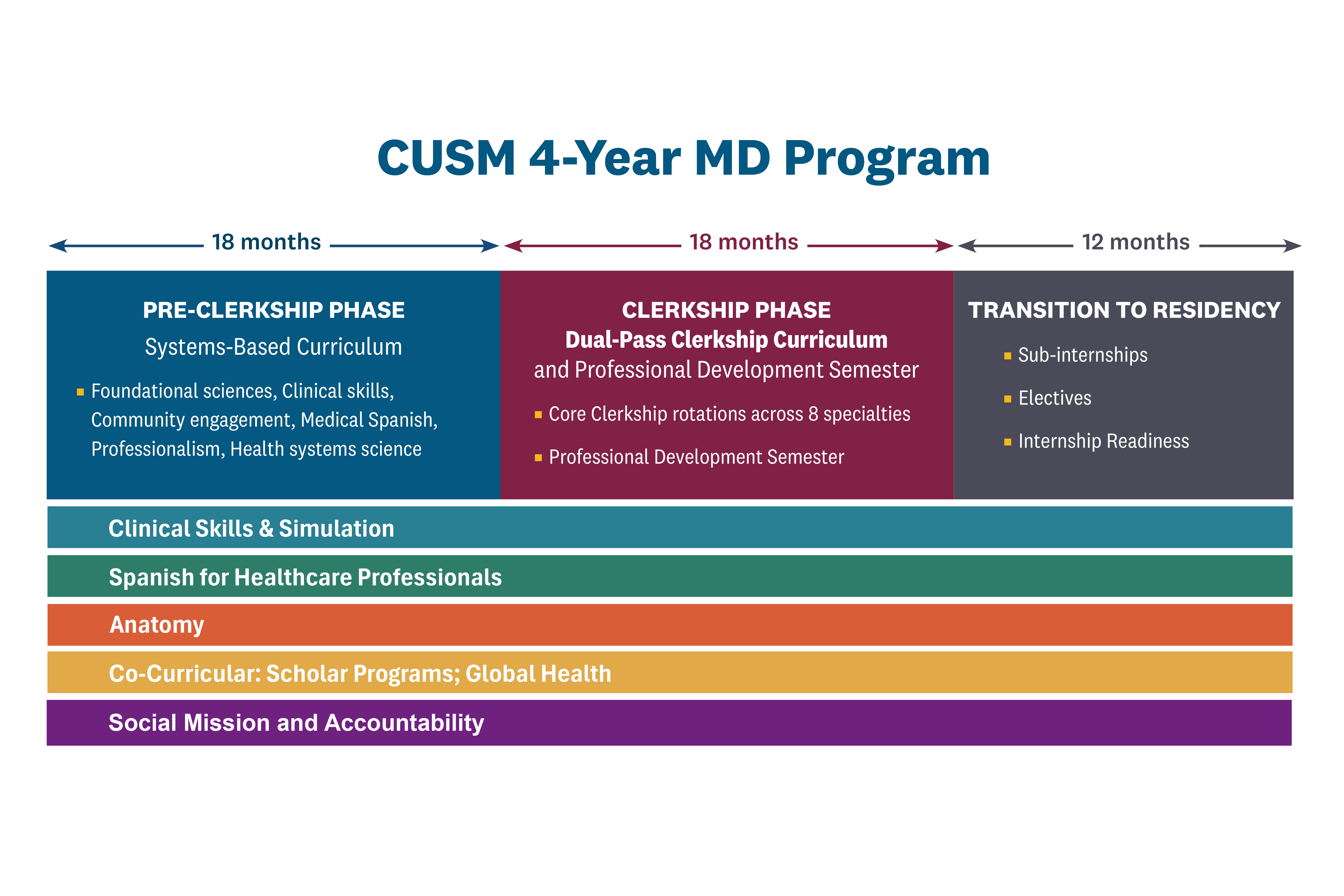
The CUSM MD curriculum is a 4-year program of study to prepare each student for a career of service in healthcare. The curriculum promotes critical thinking, teamwork, and early patient contact, facilitates the integration of basic science with clinical problem-solving, and stimulates students to develop skills for self-directed learning. The basic science and clinical disciplines are integrated with case presentations in each system from the first day of class.
CUSM MD Program Phases:
Orientation
The CUSM MD program begins with a two-week orientation program in July. Orientation is an introduction to the program, faculty, and fellow students. The program culminates with the White Coat ceremony. During orientation, students will be introduced to their small group learning communities designed for team-based learning in a flipped classroom model.
![[A sample snapshot of CUSM MD Program Construct ] [A sample snapshot of CUSM MD Program Construct ]](/_resources/images/_events/white-coat-ceremony/White%20CoatClass%20of%202027_group%20photo_1.jpg)
Pre-Clerkship Phase
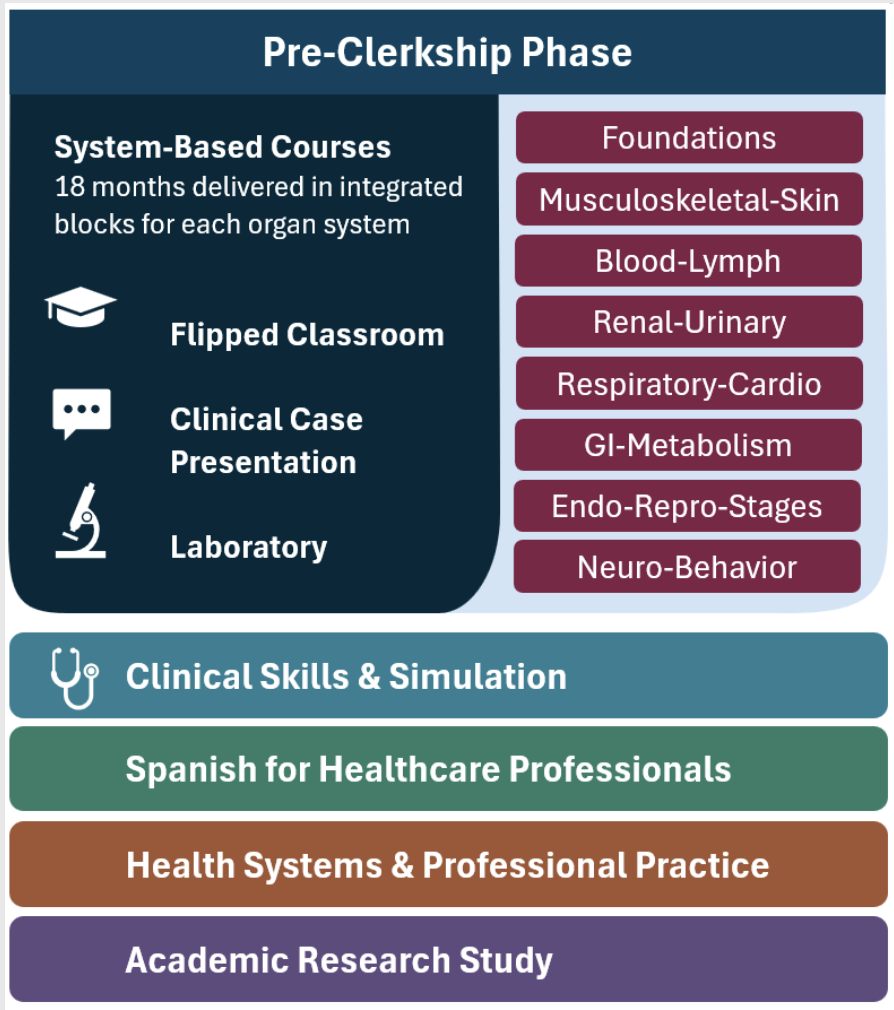
The first 18 months of the program focus on core medical education. During the Pre-Clerkship Phase, the curriculum is interdisciplinary and systems-based, with integrated coursework in the foundational sciences categorized by organ systems. Weekly, team-based clinical case presentations within the Systems courses promote application-based learning and the development of clinical reasoning skills. These activities are aligned with weekly Clinical Skills sessions that include clinical simulation and encounters with standardized patients. Health Systems and Professional Practice coursework covers health systems science, public health, ethics, professionalism, and related topics. As part of this coursework, students participate in community-engaged projects with regional partners through the CHANGE program. In the longitudinal Academic Research Study coursework, students develop a research proposal in Year 1 and carry out the proposed study in Year 2. Students are also enrolled in a Medical Spanish course designed to build communication skills and cultural competency to enhance care for Spanish-speaking patients.
Clerkship and Transition to Residency Phases
The clerkship phase of the MD program is designed to build on the pre-clerkship experience. It includes 12 months of core clerkship rotations and a 6-month Professional Development Semester (PDS). The PDS provides the opportunity for students to explore their professional identity and engage in activities that are aligned with their professional interests, including flexible time to engage in distinguishing activities, or dedicated study time for USMLE Step.
CUSM is affiliated with Arrowhead Regional Medical Center (ARMC), which is the primary teaching hospital for the clerkship and transition to residency phases. CUSM also has several regional affiliated clinical sites that provide clerkship educational experiences for the 3rd and 4th-year students. This diversity of sites provides students with varied clinical environments to develop expertise in managing patients from a wide range of backgrounds.
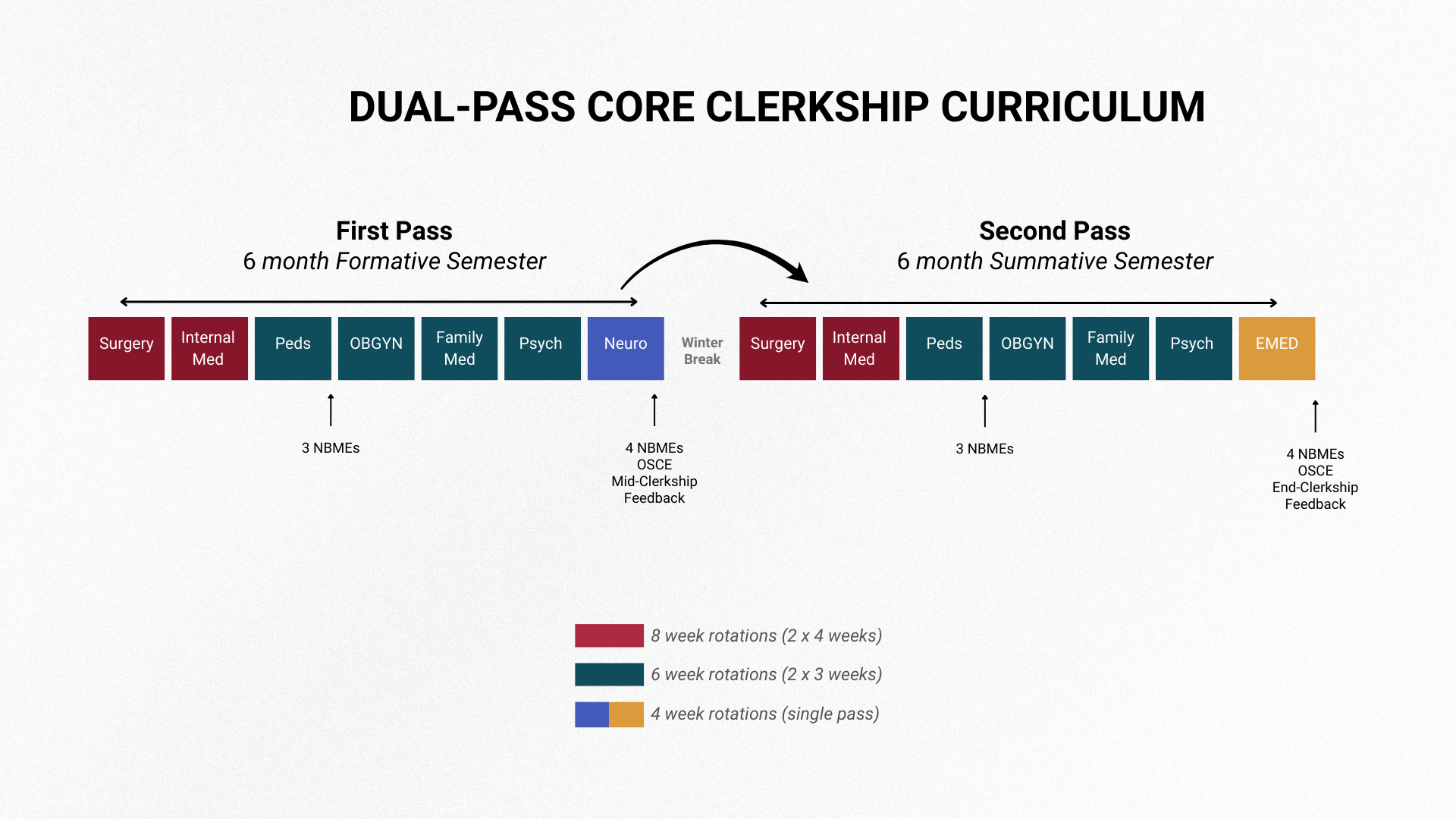
The Dual-Pass Clerkship Curriculum (DPCC) spans a full academic year, providing students with valuable experiences across multiple specialties. DPCC consists of two 6-month semesters, with students repeating 3-4 week rotations in six of the eight core clerkships. Two core clerkships, Emergency Medicine and Neurology, are single-pass, 4-week rotations.
During their first semester, students rotate through the formative first-pass of clerkships, providing a chance to acclimate to clinical environments and their roles within healthcare teams. At the midpoint of the year, students review multiple modalities of mid-clerkship, formative feedback during a 1:1 with a Clerkship director including scores on NBME, OSCEs and clinical performance evaluations.
During their second semester, students return for a summative second-pass rotation to demonstrate their clinical competence, applying what they learned during the formative semester across all dual pass specialties.
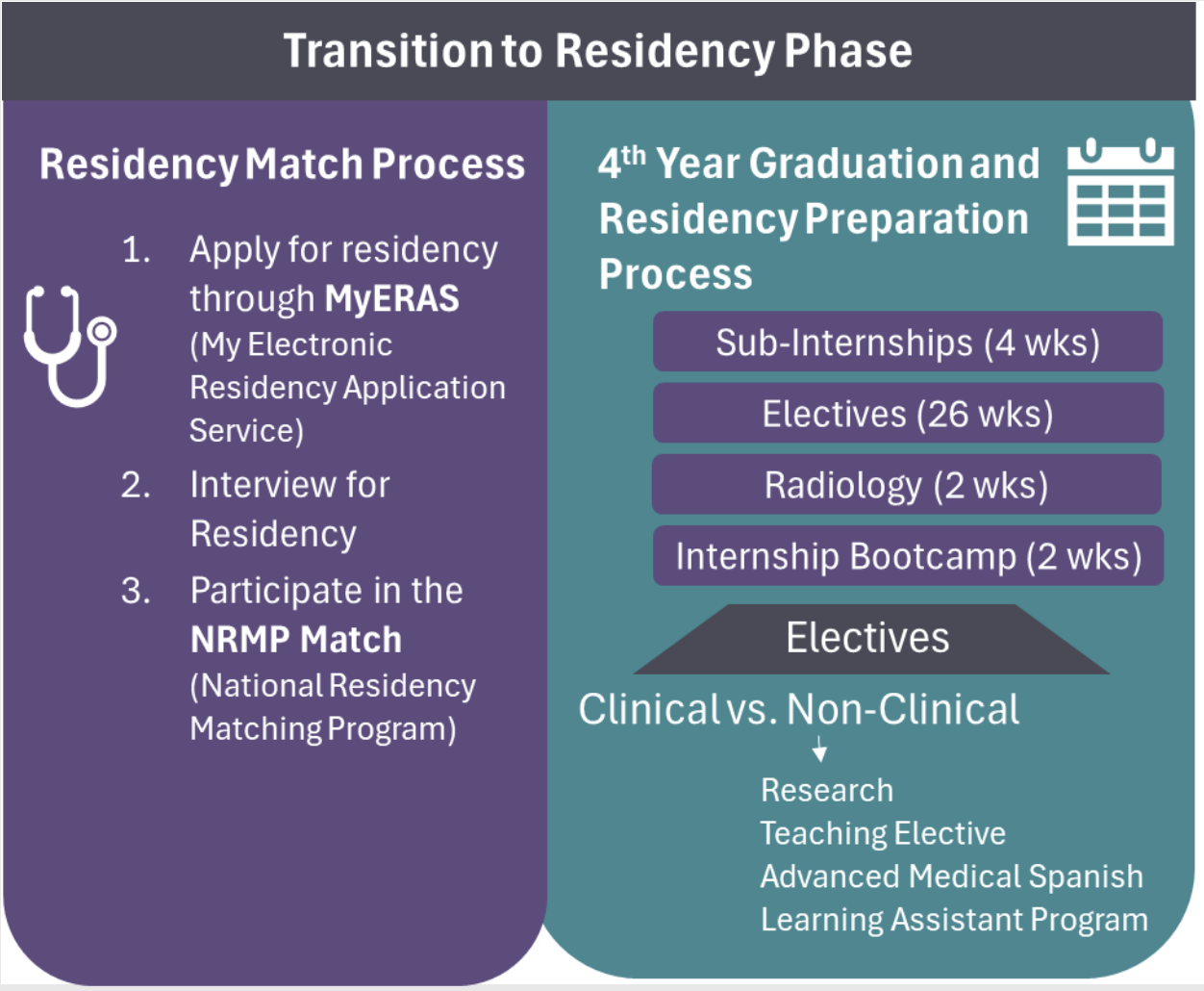
The Transition to Residency Phase aligns with students fourth year of the program. During this year, students engage in sub-internships, clinical and non-clinical electives, and a transition-to-residency bootcamp course.
Clinical Training Sites
At the California University of Science and Medicine, students complete their core clinical training primarily at Arrowhead Regional Medical Center (ARMC), a major teaching hospital serving the Inland Empire. Our clinical network includes a range of hospitals, medical centers, and community-based clinics that reflect the diverse healthcare needs of the region. CUSM values its community partnerships with clinical sites as these training opportunities reflect our commitment to training future physicians who will serve local communities.
Our clinical training sites for core clerkship rotations include:
- Arrowhead Regional Medical Center
- San Bernardino County Department of Behavioral Health
- Eisenhower Health
- Inland Pediatric
- Interim Psychiatric Care
- Inland Psychiatric Medical Group
- Mission Community Hospital
- Pomona Valley Hospital Medical Center
- Riverside Community Hospital
- Riverside University Health System
- Bernardine’s Medical Center
- Talia Medical Group
- Universal Health Services
- Choice Medical Group
- Kidstrong Medical Group